The Issue: Clinical Conversation Diversity
Clinical conversations do not have a single and uniform input. A primary care visit, an informed-consent discussion about a surgical procedure, a psychiatric interview and an ED trauma resuscitation all appear and sound different - different in pace, jargon, emotional coloring, content volume and urgency to make decisions. Include telehealth audio calls, interpretered visits, and multi-provider rounds and the difference is multiplied. Conventional dictation engines or handwritten notes can hardly ensure the accuracy and clinical meaning of that diversity; AI methods seek to dynamically adapt to the contextual features of each encounter to ensure that the documentation recorded is clinically useful and legally sound. This trend can be observed in market and product reports that indicate the high adoption of AI scribe solutions and an increasing investment in multimodal clinical capture.
Speech Recognition and Conversation Capture: How AI listens
AI scribes are based on multiple technologies:
- Automatic Speech Recognition (ASR): translates audio waveforms into sequences of words. In modern ASR models have been trained on large and medical-centric corpora using deep learning (end-to-end or hybrid acoustic models), and thus recognize medical vocabulary, medication names, and acronyms with greater accuracy than general-purpose ASR.
- Speaker diarization and role detection: determines who said what (clinician vs. patient vs. caregiver) - necessary to make attributions in subjective vs. objective findings and to assign responsibility in notes.
- Natural Language Understanding (NLU) & Clinical NLP: translates the identified words into clinical terms (symptoms, diagnoses, drugs, times, test results). This layer will map free text to organized terminologies (SNOMED CT, ICD-10, RxNorm) and identifying items to be templated and billed.
- Conversation segmentation & intent detection: splits the visit into logical units (history, ROS, PE, assessment, plan) and identifies intents - e.g. medication refill request, new complaint, referral.
Performing them well integrates these layers and refines them with domain adaptation (fine-tuning on clinician speech) and on-the-fly correction loops that enable clinicians to correct the model when it misunderstands some specialized phrasing. Guides and trend analyses of industry buyers suggest that much attention is paid to ASR accuracy and powerful EHR integration in this year.
Language and Dialects Multilingual Encounters
One of the most difficult real-world issues is language variability:
- Varying dialect and accent: ASR accuracy declines with the models being trained on a small set of accents. Best-in-class AI scribers use a variety of clinician and patient voice to retrain or fine-tune models to reduce bias and accuracy discrepancies.
- Multilingual and interpreter-mediated visits AI systems can either support multiple languages or collaborate with human interpreters. Other solutions enable capture in clinician wording, as well as provide a transcript of the capture in an alternative language to that of the chart. During the mediation by interpreters, the process of diarization is paramount: the scribe has to assign the statements appropriately to both the patient and the translator.
- Cultural and idiomatic language: patients have a tendency to refer to the symptoms through nontechnical metaphors or references of cultural identity. Normalization of concepts in clinical NLU (concept mapping of feeling like a tight band around my chest-to-chest pain/ angina-like) ensures better downstream triage, coding, and decision support.
The strategy of Scribe should then incorporate varied training facts, continuous model analysis between language groups and human review processes to identify systematic errors.
An Understanding of Clinical Reasoning and Situation
A written text is just but the beginning. Clinical reasoning is found in high-value clinical notes: temporality (started three days ago), severity (severe, 8/10), trajectory (worse at night), and decision rationale (ordered chest x-ray because of persistent focal consolidation on exam). Modern AI does this via:
- Temporal and causal parsing: identifying onset, progression and cause-effect relationships in speech.
- Context-based summarization: choosing salient facts to be used in the assessment and plan instead of generating a verbatim transcript. As an example, a physician working in an ED can spend 20 minutes talking, but only several important details can be required in the final ED note.
- Evidence linking: in cases where possible, map the note to objective data (vital signs, recent labs, imaging) through EHR integration to bring the assessment and plan to be more precise.
Since AI can hallucinate or exaggerate confidence, reliable systems display confidence scores and connect facts extracted to the original snippet of transcripts - allowing rapid verification by clinicians.
Organized Products: EHR templates, SOAP, and Billing-Ready notes
Final notes should be in a structured and practical format that is expected by clinicians and billing groups. AI handles this by:
- Template mapping: filling EHR templates (SOAP, H&P, procedure notes) with the extracted information and inserting the results into the relevant fields.
- Coding and charge capture: proposing ICD-10 and CPT codes on the basis of the registered assessment and procedures. (Note: trained personnel must review code assignment; AI increases speed of suggestions, but not coder control).
- Specialty-specific customization: a visit to the dermatology center involves capturing lesion descriptions and photo references unlike a visit to the psychiatric center that emphasizes the mental status and risk assessment. AI writers give templates and libraries of phrases that are specific to the specialty.
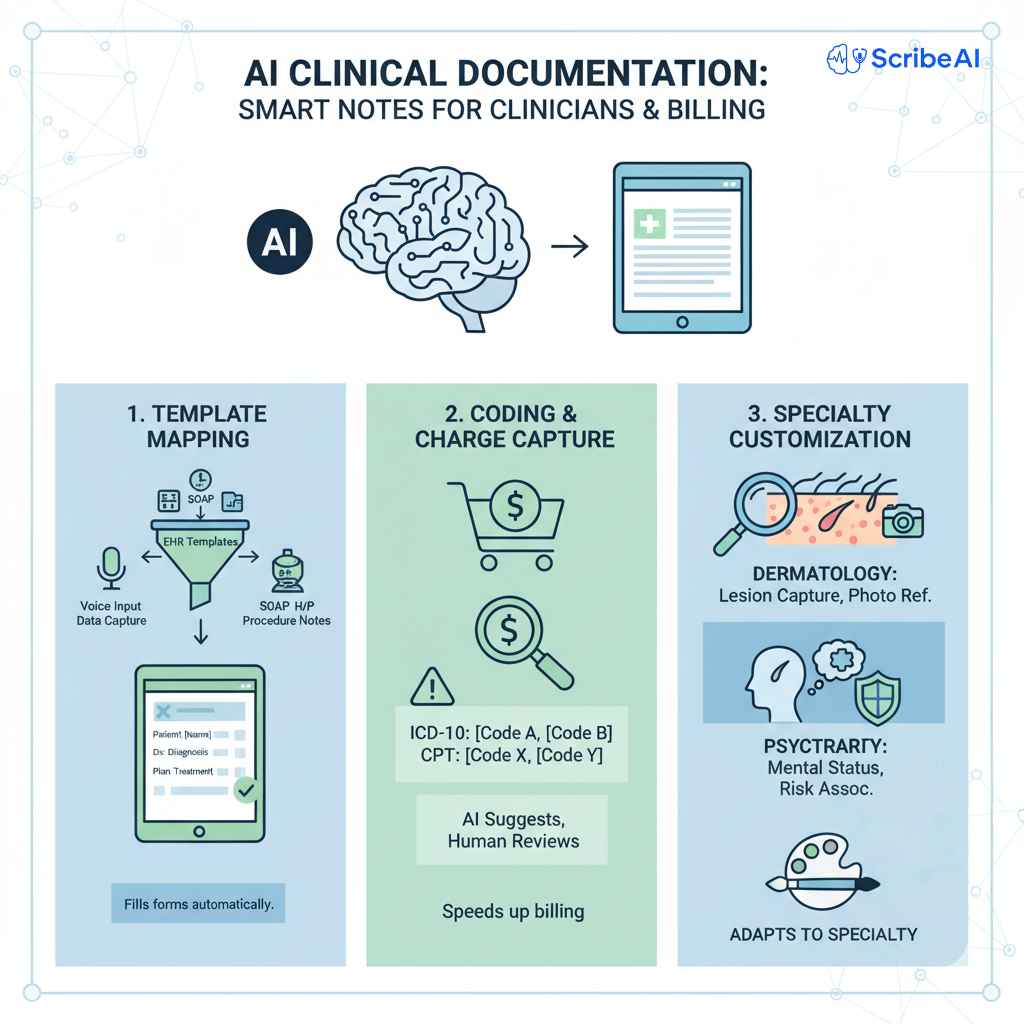
The introduction of new CPT and telehealth codes in 2025 has altered the documentation requirements in some environments; AI scribe workflows can be revised to produce supporting documentation that is in line with the existing code sets. In all cases, AI recommendations should be accompanied by clinician review to avoid upcoding and to satisfy payer documentation regulations.
Security, Privacy, and Compliance (HIPAA and beyond)
Dealing with actual clinical dialogues entails strong privacy and compliance posture:
- Data security: capture, storage, and transit are encrypted; there is a set of access controls, as well as audit recording.
- Business Associate Agreements (BAAs): any vendor of AI that handles PHI has to sign a BAA in the case of covered entities.
- On-device or private cloud processing: in certain deployments audio and inference are retained in the environment of the health system; others deploy vendor clouds with certified controls. Consider threat models and sensitivity of your patient population with deployment decisions.
- De-identification and re-identification protections: in case data is utilized to enhance models, they need to be de-identified or managed by express consent and control.
Analysis of the industry has repeatedly cited enhanced security capabilities and compliance services as a distinction between AI scribe vendors. Strictness on these matters helps to safeguard the patients and minimize legal/regulatory risk.
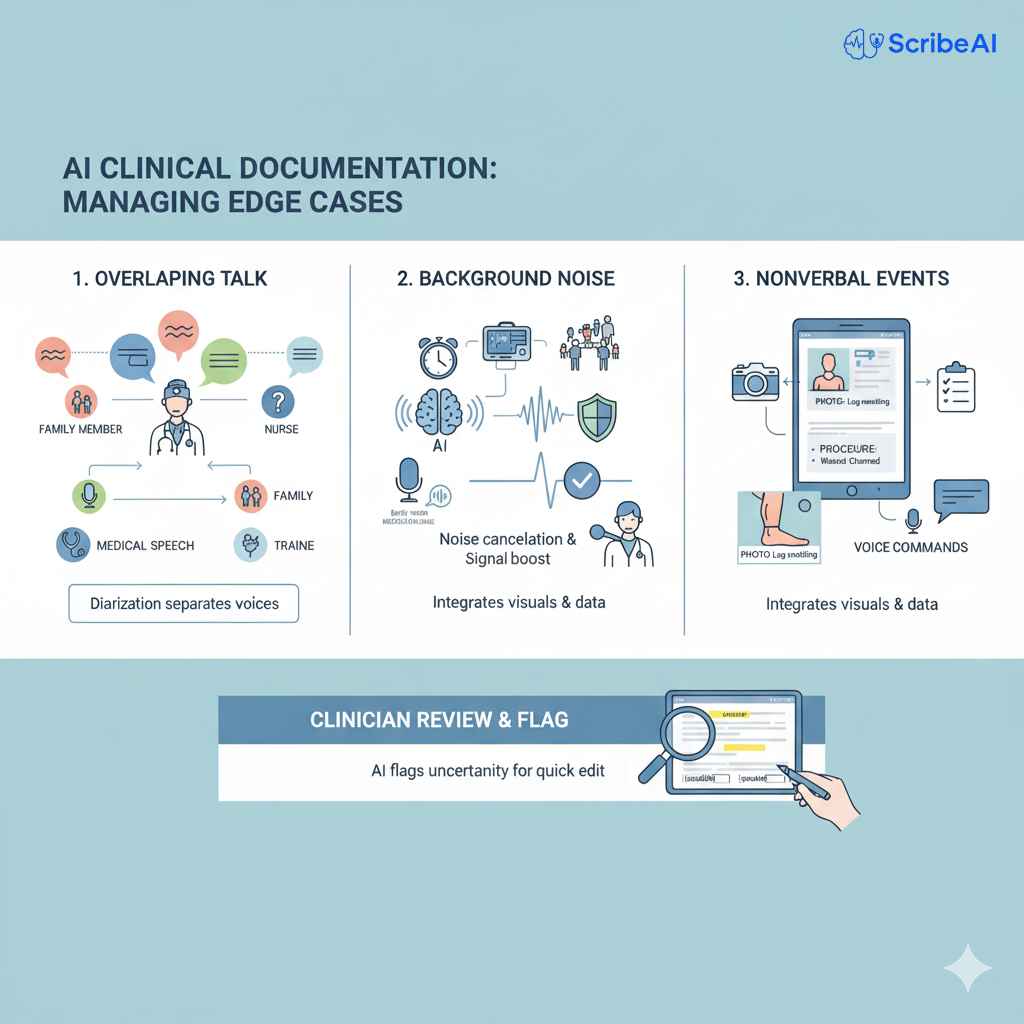
The Management of Edge cCses: Interruptions, Concurrent Speech, and Noise
There are chaos and noise in clinical settings. Edge cases include:
- Overlapping talk: the family members speak, the trainees clarify the points, the nurses report the vital rates -- diarization should not mix voices and identify the phrases which have a medical value.
- Background noise: noise in the background may be in the form of alarm, equipment, or hallway noise, which can interrupt ASR. Stronger systems perform noise-robust acoustic modelling, signal improvement and microphone arrays (or mics carried on clinicians) to enhance capture fidelity.
- Nonverbal events: physical examination, physical examination observations (massive swelling, see photo) or procedure cannot be fully represented in the audio. AI upgraded workflows allow clinicians to add pictures, organized vital signs, and procedural checklists to the note using simple voice commands.
The scribe systems must have clear place-holders and flags in cases where audio quality or diarization is lowering confidence as a way to ensure that clinicians can fastly revise and fix the record.
The Validation, Clinician-in-the-loop and Quality Assurance Process
Due to the imperfection of any model, the safest implementations require clinician supervision and systematized Question and Answer session:
- Live-time verification functions: quick edit action and live note preview allow clinicians to fix or approve results during or after the encounter.
- Post-encounter QA sampling: random audits, accuracy measures by clinician and specialty and retraining in case there is a systematic error.
- Feedback loops Since user edits were fed (with appropriate consent and security controls) back to model retraining pipelines to minimize repeat errors.
- Clinical governance: committees to establish thresholds (e.g. not all types of notes will be signed; or not all will be sent to medical staff), drift checks, and documentation (clinical and compliance standard).
This paradigm of human + AI provides the most optimal solution: speed and consistency of automation and preservation of clinician responsibility and judgment.
Beneficial and Quantifiable Health Systems effects and Improvements
The implementation of AI scribes can yield returns when handled intelligently:
- Time savings and decreased burnout: The clinicians are less likely to report after-hours charting hours and better work-life balance when documentation load is reduced.
- Enhancements in throughput: Improvement in throughput by faster documentation may be used to increase the throughput of a clinic or to decrease the waiting time of patients when scheduled and staffing adjustments are made appropriately.
- Coding and revenue cycle impacts: automatic retrieval of details related to the patient can lead to less charge being missed or an improvement of documentation completeness - although coder review must be non-conformant.
- Quality of care: clinicians have more face-to-face time with patients on less-clerical systems; a few systems have higher patient satisfaction scores.
With 2025 market analyses indicating rapid expansion in medical transcription and AI scribe markets, the company is continuing to invest due to previously established impact in their operations. Measurements and results Organizations should calculate the metrics of the baseline (time per note, after-hours EHR time, denial rates) and compare the results after the deployment to prove the ROI.
The Adoption Checklist of AI Scribes on a Large Scale
- Scribe has created a checklist which is practical and which customers can use when considering and implementing AI scribe technology: Identify objectives and measures: reduction in clinician time, quality of documentation, uplift in coding, patient satisfaction.
- Data and privacy analysis: BAA, encryption, audit logging, data retention.
- Clinical workflow mapping: where the AI scribe will be? Real-time transcription in the room, clinician-facing preview or asynchronous draft generation?
- EHR integration proof of concept: test population, discrete data mapping, and order entry.
- Pilot in representative specialty mix: to test edge cases, include high-variability clinics (behavioral health, ED, telehealth).
- Clinician training and change management: scripts, verification procedures, and pathways to escalate the unattended items.
- QA and governance plan: rates of sampling, error rate, and retraining frequency.
- Vendor security audit and reference: evidence of third-party audit (SOC 2, ISO), customer references, and update roadmasters.
Equiped with a strongly measured rollout is a way of controlled adoption, and it will also detect problems at an early stage.
AI medical scribes are not magic, but rather, well-crafted piles of ASR, clinical NLP, and workflow integrations; they are developed to handle a fundamental healthcare issue, which is that clinical conversations are incredibly varied. AI can dependably translate conversations into clinically useful, billable notes when trained on varied training data, with robust privacy controls, clinician-in-the-loop validation and with specialty-sensitive templates, reducing clinician burden and enhancing operational metrics.
You can try a pilot of clinician-first, privacy-focused solution, with lots of flexibility to accommodate various clinical needs, at Scribe, should you be comparing AI documentation to your practice or health system.
Frequently Asked Questions:
Q1. Do AI scribers work well enough to be able to displace human transcriptionists?
Not entirely. AI scribers greatly save the time spent by clinicians in writing, and are capable of generating high-quality first drafts, although best practices maintain clinicians or certified reviewers in the loop to write billing-sensitive or legally meaningful documentation. With specialty-specific tuning and QA over time, AI accuracy on common encounters can be equal to that of human-assisted processes, although there is a concern about the vendor used and its governance.
Q2. Does AI scribe support telehealth and audio-only visits?
Yes. A large number of AI scribe systems are telehealth capture friendly and have been revised to include new telemedicine coding and documentation rules that were added in 2025. The process of integrating EHR with telehealth visits and the clear expression of a visit modality is pertinent in compliance.
Q3. What is the privacy protection of AI systems on behalf of patients?
Control services are offered by vendors (encryption in transit and at rest, role-based access, audit logs), and contractual services (BAAs). There are deployments that continue to process healthcare infrastructure; deployments that seek vendor clouds that are certified (SOC 2, ISO 27001). Before onboarding, verify the vendor security posture and security retention.
Q4. What are the best specialties to use AI scribes?
There are immediate efficiency improvements in primary care, urgent care and highly documented specialties (cardiology, orthopedics). Comprehensive summarization characteristics characterize behavioral health and multifaceted consults. Perioperative environments and ED require structures constructed on interruptions and talk overlap. It is advisable to pilot in a wide range of specialties to get to know the variation of ROI.
Q5. Will there be a difference in billing or audit risk with AI scribes?
AI may enhance the completeness of documentation and coding recommendations, but it will not remove audit risk, unless it is supported by governance and verification of clinicians. The documentation must belong to clinicians; AI should be used to reveal supportive information but not forcefully claim the level of billing without examination.